Organise or die
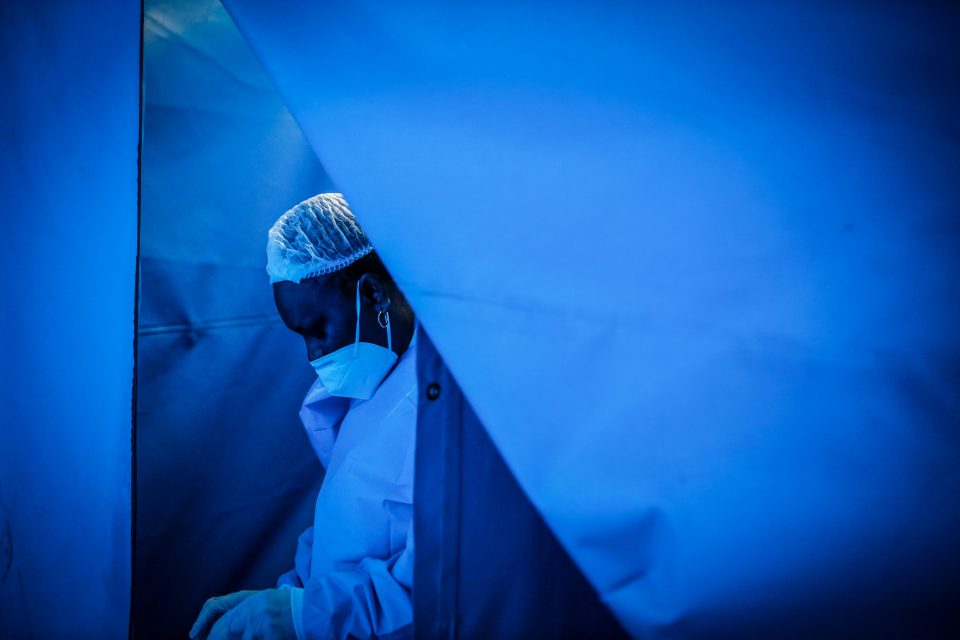
The Covid-19 pandemic hasn’t brought South Africa’s health system to its knees. Instead, it has simply exposed on a wider scale the systematic failures that were already there.
Author:
25 June 2021
For any government claiming to be even moderately progressive, public healthcare must be at the centre of its programme. However, with the notable exception of the antiretroviral (ARV) drugs rollout, the ANC has not provided adequate healthcare and has now driven the system into a severe crisis.
In the Eastern Cape, it is no exaggeration to speak of the crisis in terms of a collapse. In Gauteng, the closure of the Charlotte Maxeke hospital pushed an already strained system over the edge. People are dying in hospital corridors and foyers, and in ambulances parked outside in long queues.
In all provinces apart from the Western Cape, the vaccination rates for Covid-19 are less than 1%. Elective surgeries have been cancelled in private hospitals, there are no intensive care unit beds in Gauteng, babies are dying in the Eastern Cape’s neonatal wards and the health minister is on special leave after being connected to a rotten tender.
Related article:
Many impoverished and working-class people have already lost breadwinners. At the same time, the number of people needing support from those who still have jobs has increased because their family members lost their jobs during the lockdown. Frontline retail and factory workers often tearfully describe how, despite being employed, they and their families are surviving on meagre rations of processed carbohydrates. These are hard times, very hard times, and unnecessarily so.
Colonial medicine has an unspeakably grim history around the world. In South Africa, that history culminated in the figure of Wouter Basson, “Doctor Death”. But it was always countered by committed, decent and often brave nurses and doctors. Biomedical medicine has a dual history of functioning as a tool of oppression and as a technology of universal care, sometimes allied to emancipatory struggles.
It was widely assumed that the ANC’s ascent to state power in 1994 would result in massive investment in public healthcare and the development of a people’s approach to medicine – of the sort developed by progressive nurses and doctors in the 1980s, in the mobilisations at the turn of this century and advocated by Harvard physician Paul Farmer.
Choosing quackery and death
This was not to be. The first major crisis in the healthcare system under the ANC was the result of an ideological failure to develop a credible anti-colonial approach to medicine. Instead of drawing on the well of progressive medical history at home and abroad, not to mention the shining example of the achievements of the Cuban state, the ANC turned to the failure of Jabulani “Mzala” Nxumalo, one of its key intellectuals in the late 1970s and throughout the 1980s, to move beyond colonial Manichaeism. In 1988, writing in the ANC journal Sechaba, Nxumalo declared that HIV had been concocted in the “laboratories of the military-industrial complex of the USA”.
In 1997, as the Aids pandemic took an increasing toll on society, the ANC turned to outright quackery. This was promoted by Olga Visser, a con artist. Thabo Mbeki and Nkosazana Dlamini Zuma backed virodene, Visser’s snake oil that was primarily composed of dimethylformamide, a highly toxic industrial solvent, as pharmacotherapy.
Mbeki embraced Aids denialism the following year, setting the stage for hundreds of thousands of people to succumb to needless and painful deaths. His denialism was enthusiastically embraced by Manto Tshabalala-Msimang, a medical doctor, and regional apparatchiks such as Neliswa “Peggy” Nkonyeni in KwaZulu-Natal.
Related article:
The tide began to turn in 1998 with the formation of the Treatment Action Campaign (TAC), led by Zackie Achmat, one of the most significant political figures to emerge in post-apartheid South Africa. The TAC worked with doctors and scientists, as well as trade unionists and grassroots activists, to build the most important popular health movement on the planet at the time.
The era of denialism was over by 2008 and the state began to move towards providing life-saving antiretroviral medication. Today, millions of people access ARVs through the public health system. It is an extraordinary achievement, won by popular organisation and mobilisation and the progressive scientists and doctors who offered their support to that struggle.
Corruption that sickens and kills
The possibility of the gains won in struggle enabling further progress was soon threatened by corruption. This hit KwaZulu-Natal particularly hard in 2009 when Nkonyeni, who was still the member of the executive council for health at the time, was responsible for a corrupt and wildly excessive tender to procure and maintain radiotherapy machines. Most of the oncologists working in the public health system in the province resigned because they no longer had the material means to practise medicine effectively. Cancer treatment completely collapsed in public hospitals and, again, people were dying agonising deaths that, in many cases, were entirely avoidable.
As Jacob Zuma’s government turned into a full-blown kleptocracy the problem of corruption became systemic. The healthcare system – like public transport, housing, electricity provision and the state’s land reform programme, such as it was – became a site of organised plunder.
The Gauteng Department of Health began to “deinstitutionalise” psychiatric patients in 2015. In what became known as the Life Esidimeni tragedy, 143 people lost their lives. Some were left naked; some died of hypothermia, dehydration and starvation. Like the Marikana massacre in 2012, this was no “tragedy”, no disaster created by some act of God. The patients were removed from public healthcare and left to die, often in the interests of private profit.
Related article:
The plundering of the healthcare system by a kleptocratic political class has continued under Cyril Ramaphosa. The nation was left reeling in 2020 when it became clear that there had been a massive looting of the funds allocated to deal with the Covid-19 pandemic. The ANC went on to bungle the vaccination programme, leaving millions unprotected. The failure to adequately invest in hospitals and maintain them to an appropriate standard appears to have led to the fire at Charlotte Maxeke.
In the early months of the Covid-19 pandemic, doctors such as Salim Abdool Karim and Minister of Health Zweli Mkhize became trusted figures. When Mkhize’s complicity in the plundering of the initial budget allocated to develop a national health insurance system came to light, South Africans reeled from yet another shock.
The ANC’s destruction of public healthcare began with a warped anti-colonial ideology, was effectively contested by popular mobilisation, and then rapidly escalated because of kleptocracy. It now faces a third phase in its degeneration: the programme of austerity driven by Ramaphosa’s faction of the ANC.
The insanity of austerity
Respected economist Duma Gqubule has spoken of “the insanity of the government’s austerity policies” and noted that “they have announced cuts of R50 billion from the health budget over the next three years in the middle of a pandemic”.
There are no objective constraints on the ANC’s capacity to build a healthcare system that receives people with dignity and effectively meets their needs. After all, Cuba has built an extraordinarily good healthcare system and offered medical solidarity to countries around the world, even though it is not a wealthy country and has endured a United States blockade since 1960.
Related podcast:
The achievements in Cuba are in striking contrast to the situation in many capitalist countries, where governments refuse to fund their public health systems at a level at which they can adequately care for patients in a pandemic. Outside of the social democracies, the standard approach is to provide the lowest amount of funding necessary to cover hospital services such as emergency and intensive care, acute heart surgery and maternity care.
Waiting lists quickly build up for essential health services such as ophthalmology and hip replacements. Physiotherapy is difficult to come by, and biopsies and colonoscopies in a public hospital can take a few weeks to schedule. Under these conditions, a pandemic quickly pushes health systems into crisis.
Some of the problems in our healthcare system are not unique, but they are exceptionally severe.
At the core of the crisis
It is essential to understand that the problem in South Africa is not a question of money or capacity. It is certainly not a question of incompetence. On the contrary, the ANC is highly skilled at doing what it actually wants to do. The problem is simply a question of political will.
As we saw during the Aids pandemic, effective organising can force the ANC to generate the required political will to address health issues. This is a central task of our times. The news of the looting of Covid-19 funds and then the scandal around Mkhize plunged many into cynicism. But we should recall our great tradition of progressive medical students, nurses, doctors – and ways of practising medicine.
Related article:
Some of this is well known. For instance, Aubrey Mokoape, a key figure in the emergence of the South African Students’ Organisation in 1968 – and with it Black Consciousness as an organised project – was a medical student who went on to be a doctor. Some of the revered martyrs of the liberation struggle were medical people. Steve Biko had been a medical student before he was banned in 1973 and then murdered in 1977. Neil Aggett, the trade unionist and doctor, met his death in police custody in 1985. Victoria Mxenge, assassinated in the same year, was a trained nurse. Abu Baker Asvat, the people’s doctor, was murdered in 1989.
But there is also a much longer and older tradition. For instance, in 1908 Cecilia Makiwane became the first African woman to be registered as a professional nurse. She worked with great dedication at the Lovedale hospital for many years. Makiwane was a key participant in the first women’s anti-pass campaign in 1912. Dora Nzinga began her nursing career in New Brighton in 1919, served with similar dedication and became known as the “Mother of New Brighton”.
The ANC spits on this legacy and spits on the lives of the people in whose name it rules. In this crisis, as in others, it is time to organise. To organise or, for some of us, to die.





